Treating Torn or Broken Down Menisci
When meniscus repair is not possible or practical,
surgically removing either acutely (freshly) torn or chronically
broken-down meniscal tissue with an arthroscope usually provides
satisfactory relief from the joint pain and locking / popping
caused by the defective meniscus. Sometimes the pain relief is
incomplete, however, since the knee has not really been structurally
restored to normal and the joint surfaces themselves are subject
to becoming tender (if they weren't already). Secondary measures
may then need to be taken, in some cases including the surgical
insertion of an allograft (transplanted replacement) meniscus
into the knee joint. While meniscus transplants often prove
helpful in relieving chronic pain in a non-arthritic knee that
has lost a meniscus, it has not yet been proven that transplanted
menisci prevent or reduce future knee arthritis in humans. For
that reason, meniscus transplantation in a knee that seems to
be doing fine despite having lost one of its menisci is controversial
and only rarely done.
When a previously healthy (non-degenerated) meniscus is traumatically
torn in a repairable (vascular) zone, repair methods may
take several forms. Sometimes very peripheral tears of the rear
section of the medial (inner side of the knee) meniscus are best
repaired by way of "open" (non-arthroscopic) surgery,
using a skin incision that can be kept as small as 1 1/4 inches
in length. A secure and anatomically accurate suture repair can
be performed through such an incision. Most other repairable meniscal
tears are treated arthroscopically, using guided meniscal suturing
techniques (see FIGURE 4) or repair
by way of bio-absorbable (slowly dissolving) meniscal repair darts.
In the latter case, a specialized insertion instrument is utilized
to pass the tiny fixation dart, pin or clip through the inner
section of the meniscus, across the tear and into the outer section
of the meniscus, thus holding both segments of the torn meniscus
together (see FIGURE 5).
 |
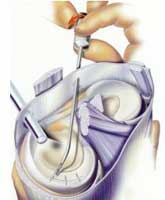
FIGURE
4 - This picture demonstrates the top portion of a
tibia, upon which are resting the medial and lateral menisci.
A peripheral, longitudinal (parallel to the meniscal curvature)
tear in the medial meniscus is shown in the process of being
suture-repaired. The femur is not shown here, so as not to
obstruct a full view of the menisci. Note that the tear is
relatively even and linear, and located in the outer 1/3 (or
so-called "red" zone) of the meniscus, which makes
it ideal to repair. Tears in the inner, thinner 2/3 of the
meniscus (immediately to the left of the tear shown here)
would be far less likely to heal if repaired because this
portion of the meniscus does not have a capillary blood supply.
|
 |
| FIGURE 5
- Diagrammatic illustration of an arthroscopic meniscus repair
technique using bioabsorbable (slowly dissolving) meniscus
repair darts or "arrows". |
The general internal environment of the knee at the time of repair
seems to have some effect on the chance for successful meniscus
healing after surgery. It has been found that meniscal repairs
done at the same time as surgical reconstruction of the anterior
cruciate ligament have a somewhat better chance of long-term success
than meniscal repairs done by themselves. This may be due to biochemical
healing factors that are more active within a knee joint that
has been irritated in a more extreme fashion by way of more extensive
injury and surgery.
Aside from good surgical technique, the key to obtaining a high
success rate with meniscal repair is often as simple as using
selective judgment when making the decision to repair versus remove.
All possible effort should be taken to repair otherwise healthy
menisci that have excellent healing potential, whereas effort
should not be wasted on thoroughly degenerated menisci that have
no realistic chance of healing well and/or functioning normally.
The decision whether or not to attempt repair in a "borderline"
case (i.e., adequate healing is unlikely but not impossible) can
involve some input from the patient, as well as consideration
of the patient's specific circumstances. The younger
the patient, the more consideration should be given toward meniscal
repair, as loss of meniscal function sets in motion an accelerated
aging process within the joint that leads to at least some degree
of future osteoarthritis in the affected region of the knee. In
an older individual (over 35 or 40) who is not
overweight and who has no leg malalignment ("bowleg"
or "knock-knee" deformity) a "borderline"
meniscal tear with a sub-par chance for healing after meniscal
repair is often best treated by primary meniscectomy. This is
because the patient's knee has probably already
been subjected to the majority of stresses that it will see during
the course of its lifespan, and it has no specific risk factors
(other than the meniscus injury) for premature osteoarthritis.
This makes the loss of meniscal cushioning less objectionable.
One must also consider the greater risk of surgical complications
associated with meniscal repair procedures (vs. simpler and quicker
removal procedures) and the extra surgical risks that the patient
would be subjected to if a second procedure were
to be required because the repair of a "borderline"
tear ultimately failed. Even under ideal circumstances, a surgically
"repaired" meniscus is not guaranteed to heal!
When deciding whether to repair or remove problematic meniscus
tissue, each patient's case must be considered individually, taking
into account the patient's circumstances and wishes, the degree
of pre-existing meniscal degeneration evident, and the overall
physical condition of the knee at the time it is first inspected
arthroscopically. Your surgeon's knowledge and expertise are also
important!
|